All you need to know about FUE hair transplant.

For an experienced, specialized and moral hair surgeon, the FUE (Follicular Unit Excision) hair transplant technique is a very useful “tool” that allows him to help his patients even more and especially those who might have previously been considered unsuitable for Hair Transplant.
As a hair surgeon, I value the FUE technique as it has helped many of my patients regain their hair and confidence.
However, like any other tool you need to know how and especially when to use it.
An old saying goes “if all you have is a hammer, everything looks like a nail.”
In recent years, some hair surgeons who have been perceived by patients as rock stars have appeared on the Internet and in several Hair Loss Forums.
These hair surgeons present the FUE Hair Transplant technique as “the one and only way” and as the “unique modern hair transplant technique”. All of them are powerful opponents of the FUT Hair Transplant technique and have a lot of patients on their side, since they have actually helped many patients by correcting the bad old transplants that had been done to those patients.
Without any exception, these hair surgeons have “discovered” and sell one or some of the special tools or machines used in the FUE technique by other doctors, and their entire scientific reputation and prestige is based on the FUE technique.
In such cases, the patient should be very careful.
I will present to you below, the scientific, well-documented and balanced truth about the advantages and disadvantages of FUE hair transplant technique, but mostly I will explain to you when it should be applied and which patients are not good candidates for the FUE.
Note
As a certified hair surgeon I use all the official hair transplant techniques, FUE, FUT and BHT (Body Hair Transplant) since 2004.
Evidently, I do not sell any “made-up” tool I have created or a special machine for a specific hair transplant technique and neither I have come up with my own “exclusive” hair transplant technique.
Basic Concepts of the FUE
The methodology of FUE evolved from the same principles of circular Standard Punch Graft extraction that were introduced back in the early 1960s.
What is the FUE technique and its procedure?
FUE is a delicate procedure that requires high-power magnification and uses small circular high-quality trephine punches, less than 1mm in diameter, to “cherry-pick”, isolate, and in situ extract individual follicular units. The punch is mounted on a manual handle, on a motorized hand device, or a robotic device.
The FUE harvesting process leaves a circular wound or incision, which heals by secondary intention, leaving a tiny scar that remains mostly inconspicuous even with a very short haircut.
The procedure has achieved increasing popularity as compared to FUSS since there is no linear donor scar, and patients falsely consider it as “minimally invasive”, “scarless”, and “painless”. It has also found greater appeal among new hair surgeons since the barrier of entry of necessary previous surgical skill, experience, and staff resources needed for successful FUSS (Follicular unit strip surgery) seemed much lower.

The restrictions of FUE
Sadly, the perceived wisdom of a less invasive and “easier” procedure has overwhelmed the reality of the extended training, long learning curve, patience, excellent hand‐eye coordination, dexterity, scientific knowledge of hair anatomy, distribution, and angulation required to pursue skilled FUE donor harvesting.
FUE is an extremely time-consuming surgery that is variable and very patient-dependent, requiring focus and experience as well as dedication, devotion, and enthusiasm. the FUE process also becomes
Unlike false claims, FUE is not a “scarless” but instead a “scar-spreading” technique, creating a much larger wound surface per harvested graft than FUSS, also necessitating harvesting from “unsafe” donor areas. It has also attracted criticism as it results in a greater transection of hairs. Success in FUE depends on the customization of each procedure for the individual patient.
The FUE nowadays
The technique has both numerous advantages and disadvantages for the hair surgeon and patient but the benefits alone have taken on a favorable “aura” for potential patients and for those who would never have considered having a hair transplant.
FUE is a valuable addition to the hair restoration surgeon’s armamentarium, and the whole HRS industry has boomed in the last decade, primarily due to FUE. This boom has resulted mainly from the advertisement done by the FUE machines marketing companies and by neophyte doctors trying to avoid the hardship of learning the techniques of proper dermatologic surgery. An increasing number of physicians and most of the new physicians are now offering FUE exclusively, but the quality is questionable in most practices.
Unfortunately, this great progress has been darkened by the perversion of unscrupulous practitioners and entrepreneurs who commoditized the FUE technique and HRS field. They treat this complicated and nuanced procedure as “not even surgery” and delegate it to unlicensed technicians who have no idea what they are doing, will operate on anyone, and are already creating a new generation of unhappy patients.
An early “disclaimer”
The FUE technique has revolutionized the HRS field in numerous ways. The estimated worldwide market size of Hair restoration Surgery (HRS) has boomed; from a global value of 1.2 billion $ in 2007, it has reached more than 9 billion $ in 2018. This has been driven by the increasing demand for FUE that has been (falsely) marketed as “minimally invasive”, “scarless”, and “painless”. All these seem to take on a favorable “aura” for candidates and those who would never have considered having a hair transplant. New enabling technologies and new service organizations that can assist doctors in surgery have appeared. These changes decreased the barrier to entry into the field that previously required surgical skills for strip removal.
The historical background of the FUE technique
The technique that would later (2002) be coined as FUE by Rassman et al. was not exactly original; similar ideas had been tested during the 1970s and continued to evolve even during the first years of FUSS. One can also argue that this type of blind extraction was first described by Okuda in 1939 who was using punches of 2.5 to 3.0mm diameter at the time.
During the “Punch Graft era”, hair surgeons tried to avoid the tufted look of 4mm standard punch grafts on the hairline by using smaller grafts. Hair surgeons, instead of using the standard 4mm punch, experimented with smaller punches, measuring even less than 1.5mm in diameter. Rather than merely removing small pieces of hair-bearing tissue, it was attempted to directly extract intact individual FUs from the donor area, in effect, creating grafts that were identical to those generated by single-strip harvesting and stereo-microscopic dissection. The first to publish hairline refinement using punches of 1.5-2.5mm in diameter was Pierre Pouteaux, who published his results as early as 1980. Even though he preceded any other similar technique by almost two decades, he is not considered the “father” of the FUE technique, probably because his focus was not on extracting naturally occurring FUs.
The FUSS (Follicular Unit Strip Surgery) era
During the FUSS era, surgeons wanted to circumvent the necessity of producing even the finest, undetectable linear donor incision line of graft removal in FUSS. The first to publish a successful technique of extracting naturally occurring FUs from the scalp was Inaba in his textbook in 1996. Unfortunately, soon after publication, Inaba passed away, and it was never clear whether he had been applying this technique even earlier. Inaba used 1mm punches, which he inserted down to the dermis, then would pull the follicle upwards and “dig” around it with a Pean’s forceps to detach it to avoid injuring the bulb. However, this technique was extremely time-consuming and did not become popular.
Ray Woods and Angela Campbell from Australia were perhaps the first to utilize the extraction of individual FUs from the donor area. They reportedly used their “mysterious” technique since the early 1990s and coined it “Hair Follicle Single Unit Extraction” or “Top-Up technique”. They decided to inform the public of the “Top-Up technique” in October 1995 with an ad in the Australian tabloid newspaper “Sun Herald” but did not share the nature of their technique professionally. They actually managed to keep their technique “in the closet” for several years, even though limited indirect information on the technique -by the results on their patients- did not reflect well on the inventors due to excessive donor scarring.
From experimenting to the birth of FUE
Rassman et al. had started experimenting with tiny punches since 1997, working on tools to circumvent the problem of FU transection due to “anatomic splay” (more on that later). However, variations in instrument design were not able to obviate the problem, and the mean transection rate of >30% was rightfully considered unacceptable. Even though they did not widely implement this technique, they continued working on ideas on how to overcome the problem of hair follicle transection.
Eventually, Rassman et al. published their invented technique in a peer-reviewed medical journal in 2002, and these brilliant scientists described the details of their FUE technique, its advantages, and limitations in detail. They had actually evolved the technique of Inaba and rendered it more efficient, applicable to a large number of grafts within reasonable surgical time while maintaining high survival rates.
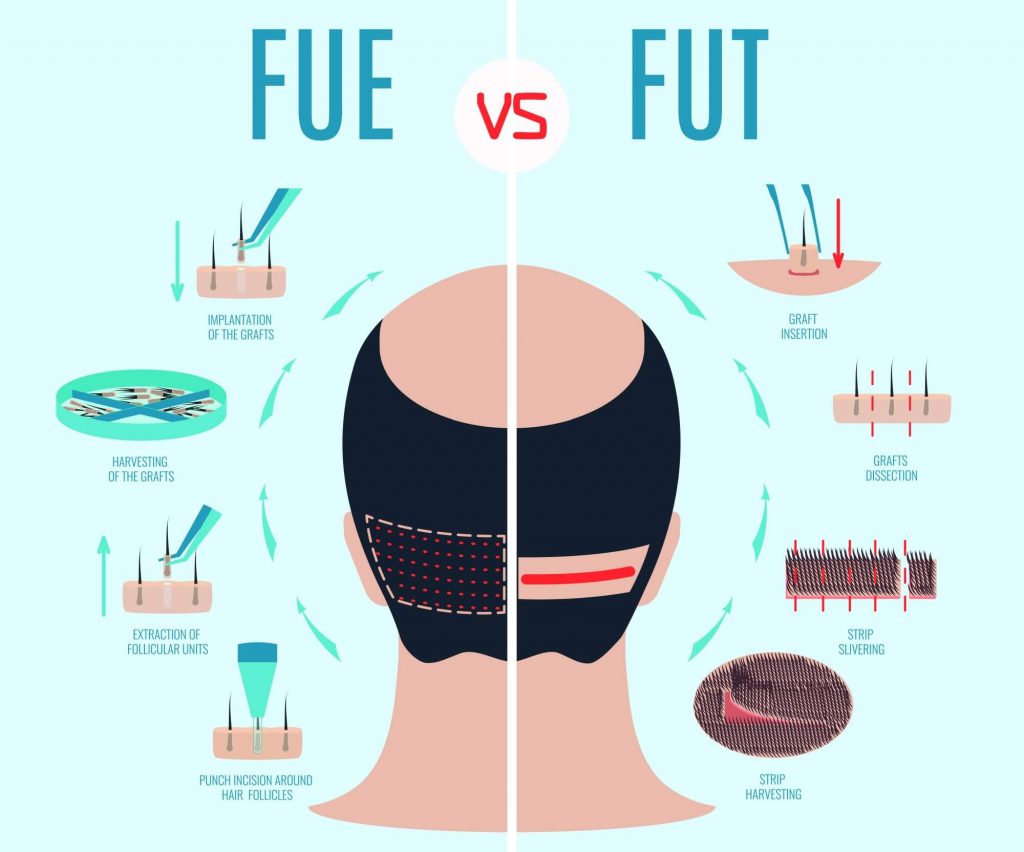
FUE vs FUT in a glance
FUs explained
Natural FUs containing 1-4 hairs are narrowest at the surface since they are gathered in a tightly bound bundle at the dermis level. However, follicles within each FU do not always follow the same path along the entire length of the grouping, and they naturally splay apart in random, unpredictable directions and angles in deeper layers. The splay of hair follicles is as important as the exit angles. Since the hair follicles splay at the deeper levels, it is less likely that all will fit into the extracting punch. Using a small punch to encompass the FU at the surface is sufficient, but as hairs diverge in different directions, advancing the punch deeper can easily result in transection of bulbs.Using larger punches to encompass all hair will cause too much injury and could not be accepted.
The prerequisites and the right process of FUE
Efficient and successful FUE donor harvest has crucial technical, surgical, and artistic prerequisites. One of the challenges in FUE donor harvesting is the variability of the donor area. The viscoelastic properties of the skin are essential in FUE and contribute to the unpredictability of donor harvesting. The tissue characteristics of skin vary among patients, and the skin’s viscoelastic characteristics impart biomechanical properties similar to the elastic properties of solids and viscous properties of fluids. The patient-to-patient variations in the epidermis, dermal-epidermal junction, and subcutaneous tissue contribute to the challenges of donor harvesting and obtaining low follicular transection rates.

Only a specialized surgeon can give you a perfect result with the FUE technique.
Advantages and disadvantages of FUE
FUE does not only promise that patients can wear their hair short without a visible linear scar. Additional proposed benefits are considerably less postoperative discomfort or pain, more rapid surgical recovery, no significant restrictions on exercise, a possible increase in scalp donor capacity (areas superior and more anterior to the ears and nape of the neck can be safely harvested, limitations imposed by scalp laxity are decreased) and expansion of the potential donor area to include body hair.
These benefits more than offset the social problems seen with the shaved donor area, which have to be managed for the first week or so after an FUE procedure. In addition, the lower barrier of entry for physicians in FUE (both in terms of perceived need for surgical skills and no need for multiple surgical staff trained in laborious microscopic dissection) has resulted in an explosion of providers around the world. Many providers wanted to enter the business but were unwilling to put together the complex infrastructure necessary to deliver a quality FUSS procedure, requiring teams of highly skilled nurses and/or technicians to dissect the grafts. With the development of the technology and more accessible FUE devices, they just jumped on the “FUE wagon” without a second thought.
Non-physicians performing FUE
Sadly, the perceived wisdom of a less invasive and “easier” procedure has overwhelmed the reality of the long learning curve required to pursue skilled FUE donor harvesting. Even worse, a large number of providers are not even physicians. Therefore, the benefits of FUE when not expertly performed by a professional, trained and authorized provider (advisedly, a physician) will come at the severe cost of reduced survival, wasting of donor area reserves, and overharvesting. Nevertheless, the “objective pros and cons” of the technique will be presented below, taking as granted that the technical skills of the physician are excellent, tools are suitable, and that artistic perception is superb.

FUE technique: Advantages and Drawbacks for the hair surgeon
| Advantages |
Drawbacks
|
| Advantage
The hair surgeon is confident that the patient will be more pleased with the image of the donor area compared to FUSS. No one can safely predict the width of a FUSS scar, especially when more than one strip harvest is required. In contrast, white dots due to FUE harvesting, if spread homogeneously throughout the donor area, produce the most aesthetic benefits. |
Disadvantage
FUE requires the hair surgeon to reengineer the fundamental processes that he/she has learned with strip surgery and will have to modify most techniques. Even hair surgeons who are very experienced in FUSS will need to learn a completely new skill, that of FUE harvesting. |
| Advantage
There is no need for a large assisting staff in contrast to FUSS surgery that requires the physician to maintain a large team of expert technicians and a big operative setup. Extracted grafts need minimal trimming and are practically ready for placement, principally when implanters are used. Therefore, an experienced hair surgeon alone or with just 1-2 assistants can complete most FUE cases requiring 1500-2000 FUs in one day. |
Disadvantage
The two most essential factors in the success of FUE are accuracy and speed, and both come with time, focus, and practice. The speed of follicle extraction is a vital aspect in FUE, but speed should not be increased at the cost of follicular safety. Speed can be achieved with experience only, and some hair surgeons can achieve safe scoring of 800-1000 grafts per hour. |
| Advantage
FUE does not require general surgical skills or skills of strip removal, which used to be a genuine barrier to entry. Neophyte hair surgeons with zero experience in surgery or HRS can learn only the FUE technique and will often market themselves as “FUE experts”. However, artistic, diagnostic, and technical skills that take many years to develop are still necessary, even if very few neophytes seem to acknowledge this. |
Disadvantage
FUE does not require previous surgical experience, but the learning curve is long. The technique is “blind”, the hair surgeon does not know in what direction the bulb is, and only experience and perfect technique may minimize follicular injury. The hair surgeon must constantly validate successful follicular extractions microscopically at the time they are done. |
| Advantage
Anyone can be a candidate for FUE. Especially in patients that were deemed further inoperable due to reduced laxity after several HRS procedures, an experienced hair surgeon can easily harvest a large number of FUE grafts. Interestingly, reduced laxity, an objective liability in FUSS, actually facilitates FUE harvesting, and patients with tight or tough scalps are the best candidates for FUE. |
Disadvantage
FUE harvesting can be very time-consuming and needs more of the physician’s time as compared to FUSS. Since only one person can harvest at a time, only after years of practice, one can hope to extract and collect more than 800-1000 grafts per hour. Techniques of serial scoring by the hair surgeon and immediate harvesting by an assistant have been presented but require the assistant to be equally skilled and experienced as the hair surgeon. |
| Advantage
The hair surgeon can “cherry-pick” grafts according to needs. The hair surgeon can choose as many thin, single hair grafts to reconstruct a feathery hairline or mostly 3 and 4 hair grafts to offer a thicker result than an FUSS session with the same number of grafts. Moreover, the hair surgeon can pick black hair as compared to white hair, or thick/curly hair to further enhance the visible results without increasing the number of harvested grafts. |
Disadvantage
FUE harvesting is a tedious procedure that takes its toll on the hair surgeon’s patience, energy levels, muscles, and enthusiasm. The hair surgeon repeats the same movements thousands of times, must look through high magnification and intense LED light for hours while his/her patience and passion for surgery are tested. |
| Advantage
Due to the tiny size of incisions and scars, serious complications, such as scalp necrosis, are rare. Unlike FUSS, overharvesting due to misjudgment or excessive cumulative donor trauma will not present as acute, painful, and severe complications (wide/visible scarring, wound dehiscence, wound necrosis, hypoesthesia) that frighten patients. FUE donor area complications will mostly appear as donor area effluvium, or shock-loss. |
Disadvantage Eye fatigue sets in after a few hours and plays a role in the accuracy of extractions while limiting the time the hair surgeon can focus on the FUE process. Good optical lenses help, but it does not ameliorate the accommodation strain that many hair surgeons experience. |
| Advantage FUE can be used to repair results of older techniques, e.g., FUs can be removed from an unnaturally dense scalp flap or older punch grafts and recycled elsewhere. In repair FUE, the hair surgeon is not required to exchange an old scar with a new, and hopefully, thinner scar, as is the situation in FUSS scar repair. Older, wide, unsightly FUSS scars or other scalp scars may be transplanted with FUE grafts harvested from other areas to obtain a more pleasing scar cosmesis. |
Disadvantage
Surgical time also includes the time spent by the hair surgeon to strategically select grafts to harvest in order to ensure that an area is not over-harvested. An over-harvested donor area will have a moth-eaten, pseudosyphilitic appearance, especially when large (punches >1.0mm) are used. FUE scars typically heal by creating hypopigmented or white dots. It is unknown whether micro-scars are due to the normal healing process or a meta-inflammatory pigment reaction. |
| Advantage Finally, FUE may be combined with FUSS in cases needing the highest numbers of grafts that normally would not be possible with FUE or FUSS alone under “no tension” donor closure, including hairs anterior to the perpendicular line of the tragus. Additionally, combining FUSS + FUE and/or body hair transplant will give amazing versatility to the hair surgeon due to the expansion of the donor reserves. |
Disadvantage Judicious harvesting is more complicated than simply spacing extractions properly. The hair shaft diameter is not uniform among hairs on the same head; variability occurs even within the same area, with neighboring hairs sometimes varying by a factor of 2. To further complicate these calculations, there is variable hair density between occipital and parietal areas. This becomes even more complex for subsequent FUE surgeries as donor density becomes increasingly irregular. |
| Disadvantage The hair surgeon must master more than one FUE techniques and learn how to use more than one device and/or punch. Success in FUE depends on the customization of each procedure for the individual patient. |
|
| Disadvantage Repeated FUE sessions produce visible punctate scarring at the FUE sites, and some of this scarring extends below the skin to alter the directional growth of the FUs in the area where the FUs were removed (possibly collagen dependent).Therefore, reharvesting an area with FUE is exponentially more difficult than removing grafts from a virgin area. It is also much more difficult than reharvesting an area previously harvested with FUSS since above, and below the FUSS scar, skin and FUs are intact. |
|
| Disadvantage Diffuse thinning after excessive FUE harvesting is far worse cosmetically than a strip scar. Overharvesting will look like a disease of the scalp, and it is impossible to camouflage, unlike a linear scar that can be hidden by bangs above the scar. |
FUE technique: Advantages and Drawbacks for the patient
| Advantages |
Drawbacks |
| Advantage
If FUE is performed “lege artis”, the patient can still wear their hair short even after extensive harvesting. Punctuate depigmented scars will be hardly visible, even with a very close haircut. However, this will depend on several parameters, such as the number of grafts extracted, size of punch used, angle of attack, a correct extraction pattern, the complexion of the patient, contrast between hair and skin color, hair caliber, cosmetic density, etc. |
Disadvantage
The most important drawback is that the number of grafts that can be safely harvested over one sitting and over one’s lifetime (total donor capacity) is less when only the FUE technique is applied. This, however, is a long-term liability, and most patients will sacrifice the final number of “lifetime extractable grafts” for the exchange of no linear scar in the donor area. In order to treat advanced baldness, the maximization of grafts harvesting would require FUE sessions to be combined with FUSS. |
| Advantage
Another, very easy to believe -but not real- “advantage” of FUE is that the punctuate scarring allows the patient to have an “exit strategy” if the surgery does not give the results the doctor promised him or if he continues to lose his hair. The typical FUE patient believes that after FUE, he can still just shave his head and accept his balding fate without any signs of surgery. This is not true. Scars are always visible when hair is cut extremely short, and the only way to cover them is with very careful (and costly) SMP camouflage on the FUE scars. |
Disadvantage
The main area of concern with FUE in most hands is the higher follicular transection rate (FTR) compared to FUSS. Since FUE is a blind technique, the frequent lack of association between the exit angle of the hair and the subcutaneous course of the follicle is particularly problematic. When this is coupled with frequent changes in follicle direction, the FTR increases even further. However, with experience, the hair surgeon’s hand-eye coordination and speed will improve, the FTR will be reduced, and results can be more reliable and consistent. |
| Advantage
Post-operative discomfort is minimal, and pain in the donor area can be treated with simple analgesics. However, when a too-large punch has been used, or too many incisions have been performed, discomfort may be considerable and can last for weeks. |
Disadvantage
Extracting the grafts with strong pulling results in de-tethering with forceps, a process that denudes grafts, striping the lower portion of the follicles from their surrounding perifollicular tissues. This converts grafts into “skinny” FUs, which are considered to have a lower survival rate than “chubby” grafts. There are serious concerns about the fragility of the FUE grafts and the fact that they may be more prone to desiccation compared to FUSS grafts. |
| Advantage
Surgical recovery is rapid, downtime is minimal, incisions are typically healed in just 3-5 days, and wounds are easily concealed. |
Disadvantage
The FUE procedure is long and hence tiring for the patient. Even though harvesting of an anesthetized donor area is painless, the patient has to lie in the prone position for hours which adds to the discomfort and is boring since one cannot read or be visually entertained. |
| Advantage
There are no significant restrictions on exercise, so patients with very active lifestyles (e.g professional athletes) will safely return to their schedule very soon, in a week. |
Disadvantage
The number of grafts extracted per day is limited, necessitating multiple sessions over several days. This is a minor drawback, relevant only to patients operated in a different city or country from where they live, meaning they must stay in for more days. Successful and safe FUE megasessions (>3,000 FUs) with low FTR are provided by very few hair surgeons but are usually not recommended. |
| Advantage
Limitations imposed by scalp laxity or multiple previous donor scars are decreased. |
Disadvantage A higher cost per graft compared to FUSS is the standard since the procedure is tiring, demands great experience and specialization, and is mostly performed by the hair surgeon. Competition has led to a reduction of charges worldwide, and countries such as India, Pakistan, and China attract American and European customers with very low prices. Many clinics in these destinations offer very questionable quality of services since all steps of the procedure are fully delegated to non-medical technicians. These locations offer extremely low prices, which often consist of all-inclusive packages with hotel and transportation. |
| Advantage Additionally, scalp grafts outside the traditional Safe Donor Area (SDA) or body FUs can be harvested. However, there is plenty of controversy concerning this “artificial expansion” of the SDA. |
Disadvantage
In FUE, the entire donor area must be shaved down to 1mm (total shave) since the surface necessary to offer the same amount of grafts is 5-8 times more extensive than with FUSS. Some patients feel socially uncomfortable with a shaved look, and others are reluctant to trim their hair because scars from previous FUSS operations will show. Solutions to bypass this issue have been suggested, in which individual FUs are painstakingly harvested throughout the donor area without shaving the surrounding hairs. These include partial-shaving “tunnels” (microstrip shaving) along the back and sides of the head, each 2 to 3 cm wide, leaving the overlying longer hairs to conceal the trimmed hairs. Another idea is an individual follicular trim isolation technique, first described by Harris, trimming only those hairs that are going to be extracted. All these techniques are very time-consuming but unless the hair surgeon is highly experienced, harvested areas may be left with significant thinning. These techniques impose the risk of creating a so-called “zebra effect” or “flag-sign” scarring due to horizontal rows of scalp that are thinned out from FU harvesting which is cosmetically worse than a strip scar. Recently, long-hair FUE has been suggested to by-pass all these issues, but a small number of grafts can be extracted safely per day (<800 FUs). |
| Advantage Some experts argue that FUs that get transected during FUE harvesting will grow back in the donor area; in comparison, FUSS grafts that are injured or transected during processing are discarded and permanently lost. Nevertheless, experience has shown that injured follicles will grow thinner hairs 9-12, and that transected or buried grafts typically result in inclusion cysts. |
Disadvantage The donor area is subjected to extensive microscopic injury, as explained above. There have been reports of extensive anagen effluvium at the donor area, sometimes permanent in nature. |
| Advantage Complications due to nerve and vessel injuries are very rare. Nevertheless, there have been reports of extensive anagen effluvium in the donor area, possibly due to excessive scalp wounding and vascular compromise. In all these cases though, hair follicles are re-growing within 3-5 months. |
Disadvantage FUE on Asians will result in a lower number of potentially harvested grafts/hair compared to Caucasians due to the lower follicular density and cosmetic density. This makes FUE grafting for Asians more challenging, especially when a second harvesting procedure is needed, which will almost certainly create a see-through donor area in most Asians who do not have coarse hair. |
| Advantage Patients with extensive baldness may undergo 2 or 3 consecutive FUE sessions within a few days. The hair surgeon may harvest the occipital part of the donor area on day 1, move to the one side on day 2 and the other side on day 3. In FUSS, the donor area should not be reharvested unless 10-12 months have passed. Nevertheless, even with FUE, safe and efficient harvesting from the same region of the donor area sooner than 6 months is very laborious. |
Disadvantage Africans also have a lower follicular and cosmetic density (40% lower) than Caucasians, and since most will have unusually curly/kinky coarse hair, FUE harvesting can be extremely arduous. African FUs have a powerful “character” below the skin, with hairs splaying very abruptly and irregularly inside the skin, increasing the risk of cutting the hair shafts during the early part of the extraction process. Also, follicles form a “corkscrew” shape when removed from their in-vivo location and tend to avulse when traction is applied. Transection of the hairs in such patients is common and may not be easily overcome by traditional approaches to FUE. In patients with very curly hair, the curve of the hair must be mimicked with the motion of the punch. |
| Advantage Technician/assistant involvement in FUE can be minimal, and the patient can rest assured that the entire dissection, and even the graft implantation, are under the control of the hair surgeon. However, this does not necessarily mean that graft survival will be optimal. |
|
| Advantage Repair FUE is ideal for camouflaging old scars that cannot be removed due to extensive scarring, atrophy, and minimal scalp laxity. |
|
| Advantage FUs from other body parts may be transplanted, such as breast, back, hands, legs, genitals, etc. |
Candidacy for FUE
According to data from the ISHRS, during the decade between 2007 and 2018, there was a 10-fold increase in the number of patients undergoing FUE, whereas, during the same period, there was very little growth in the yearly average of FUSS. Evidently, FUE has opened HRS to more candidates than ever before.
Besides patients, doctors are also increasingly preferring FUE. There appears to be more of an evolution in the use of FUE going on than merely more physicians choosing FUE over FUSS. One factor among several may be that the indications for the use of FUE have been growing as physicians have improved their techniques. This has led to a concomitant increase in yield, lower transection rates, and more reliable results.

Not all patients are suitable for the FUE technique. Your consulting physician will tell you which technique better suits your needs.
Who is the most suitable candidate for the FUE?
For certain groups of patients, FUE is the most suitable harvesting technique, as long as enough FUE grafts can be harvested to meet the patient needs:
- The primary “indication” for FUE is for patients who are very conscious about having an FUSS donor scar, whether they wish to wear their hair short in the future or not. Therefore, the primary “indication” is whether the patient insists on having FUE. Some of these patients just want the “freedom” of wearing their hair short; others are terrified by the idea of strip excision, suturing, and pain, while others just want “the newest technique”.
- The younger the patient, the more suitable he is for FUE for his first HRS procedure. Young males are at higher risk for hypertrophic or wide scar after FUSS, probably due to the more “aggressive” collagen production and deposition at young ages.
- Patients with small areas of hair loss, or those requiring inherently small sessions, such as eyebrows, eyelashes, mustaches and limited areas of alopecia other than AGA.
- Patients who tend to heal with wide scars or have hyper-elastic skin (probably due to a subclinical connective tissue disease) and will probably heal with a wide or hypertrophic FUSS scar regardless of surgical skill. Notably, FUE scars may stretch in these patients as well.
- Professional athletes or those with a very active professional, personal, or social lifestyle and, those required to resume full activity soon after surgery.
- Patients required to maintain a short haircut due to the nature of their work: military personnel, law enforcement officers, firemen, actors, models, and “celebrities” may fall into this category.
- Patients with inadequate scalp laxity for a strip excision, either idiosyncratically or after previous strip surgeries, making further FUSS impossible or “inefficient” graft-wise.
- Patients with wide or otherwise cosmetically unacceptable scars that they wish to camouflage by implanting FUs inside the scar surface without removing the previous scar.
- Patients with scars from any dermatologic conditions, trauma, or neurosurgical procedures.
Contraindications for FUE
The only absolute contraindication for FUE is the limited education, training, skills, and experience of the hair surgeon who performs the procedure. Relative contra-indications are the following:
- Inadequate donor supply. Patients with a very narrow safe donor area that will not allow the extraction of an adequate number of grafts while maintaining a proper extraction pattern.
- Large bald areas needing several thousands of grafts that might leave the donor area too thin if harvested with FUE.
- Hair follicles that are changing direction unpredictably inside the dermis, mostly evident on patients with very curly or wavy hair. In these cases, the use of a blunt punch can be handy.
- Unexplained high FTR or follicular injury rate, despite correct technique, tools, and adjustments, probably due to inherent graft fragility.
- Patients with unrealistic expectations concerning coverage and having “no scars”. These are non-candidates for HRS and FUE cannot change this unless they change their perspective.
- Patients who cannot tolerate long sessions (several hours) or multiple sessions as needed.
- Patients who are not willing to trim their hair for surgery. This is the main reason why women are not good candidates for FUE.
- Patients with white hairs that are hardly visible on the surface after shaving. In this case, hair dying preoperatively can help.
- Older patients with atrophic donor area skin, which makes it difficult to isolate and extract FUs safely since FUs are too fragile.
Considerations and controversies in FUE
There are specific crucial considerations inherent to the FUE technique itself that must be considered. If a hair surgeon wishes to extract high-quality FUE grafts, minimize FTR, offer reliable results both in donor and recipient areas, and be ethical, he/she must contemplate the following:
Harvesting rationale and pattern
As explained, what makes FUE appealing, especially to younger patients, is that the hair can be worn fairly short. The essential premise is that donor area FUE scars (usually hypopigmented or white, pinpoint atrophic macules/dots) remain inconspicuous.
Since in FUE, one removes hair partially from the donor area, it is necessary to blend the white dots with remaining hair in a fashion that resembles an unharvested donor area so that surgery passes unnoticed.
In FUE, hair surgeons gradually remove one FU at a time with the intent to evenly thin the donor area while maintaining the optimal cosmesis of the donor area. To achieve that, one needs to:
- Create the smallest scars possible: punch size and angle of entry must be carefully selected on a patient-to-patient basis
- Incisions must be placed strategically: ideally, the physician must skip the neighboring FU and dissect the next one to avoid a 2 FU void, since resulting adjacent empty spaces can be visible
- If incisions are placed too close together, this produces mottling but also increases the risk of local devascularization, which could lead to scalp necrosis if it accumulates. This complication is becoming more common in patients coming from “Black-market” clinics.
The surface area that is safe to harvest from in FUE
FUSS hair surgeons harvest 100% of their grafts from within the actual Safe Donor Area (SDA) and can easily obtain 6,000 or more FUs from that area in 2 or 3 sessions. To acquire a comparable quantity of grafts, hair surgeons performing FUE only must harvest far above and far below the limits of the traditional, time-tested SDA. These are potential “danger zones” or strictly “unsafe zones” to harvest from since they contain hair (weak or strong at that moment) that will probably be lost with time. This obligatory “extended” harvesting protocol has several implications:
- The hair surgeon is obliged to leave behind thousands of the best transplantable grafts inside the true SDA to provide coverage of adjacent scars.
- Instead, the hair surgeon must harvest follicles from beyond the limits of the “safest donor area”.
- The hairs harvested from areas outside the SDA will probably be lost in the future. This means that practically, what one is offering is -at least partially- a temporary hair transplant. One could argue that this is an unethical approach since patients are promised a “permanent solution” with HRS.
- Most studies indicate that patients undergoing FUE are less than 35 years old. As future balding may encroach into a harvested donor zone that is too high or too low, the small FUE scars will become visible, and a new generation of unhappy hair transplant patients will be created.
FUE vs. FUSS grafts
FUE grafts are forcibly extracted from the surrounding tissue and typically are skinnier, with less surrounding tissue and minimal fat surrounding the bulbs. Therefore, many consider that FUE grafts are more “fragile” than FUSS and thus possess a higher risk of poor survival.
Graft quality is a significant component of FUE, and the “gold standard” remains the microscopically slivered and created grafts obtained by FUSS. Thus, the challenge for FUE harvesting methods is to produce grafts that are similar to microscopically dissected FUSS grafts.
Although the FUSS procedure, from a quality graft production point of view, probably produces a more consistent, superior graft to FUE, this technical issue seems to fall on “deaf ears” for many patients demanding FUE.
Grafts of high quality, whether produced by FUSS or FUE, must have supportive tissue throughout and be intact in all anatomical components. Only a few studies exist that compare the overall survival of FUE vs. FUSS grafts.
Overall, it seems that with experience, superior technique, and proper instrumentation, FUE grafts are not inferior in terms of quality and survival compared to FUSS grafts.
Effect of FUE on the donor area and the plague of overharvesting
The explosive worldwide popularity of the FUE has contributed to a massive increase in patients suffering donor area over-harvesting. These severe cosmetic defects range from minor degrees of visibly moth-eaten donor areas to almost complete donor alopecia. Assessing the amount of trauma that can be inflicted on the donor area and the number of grafts that can be removed with FUE before density diminishes to a point where evidence of the procedure is obvious has not been entirely determined yet. No single algorithm integrates all the various factors to predict the minimum adequate donor area density after FUE.
In addition, FUE wounds can heal with a wound size in excess of the initial punch due to angled punch entry. (Figure 10.11) Another reason is that with numerous punches, the natural contraction that would occur with second intention healing is reduced due to changes in contractile forces dispersed over a large area. Due to all these, when adjacent FUs are harvested, a space of at least 6m㎡would often be evident. When large numbers of these empty spaces are left behind, the donor area has a moth-eaten appearance (pseudo-syphilitic), with the scalp showing through hair.
This phenomenon has been coined “donor area depletion” since, besides the cumulative scar surface, subclinical vascular damage or “hidden” transections often lead to significant miniaturization of the donor hairs reducing coverage even further.
Safety of FUE megasessions
FUE mega-sessions are lately presented as modern substitutes of FUSS megasessions. Newer devices, better-designed punches, improved training, and cumulative experience -but mostly greed, ego, and ambition- have allowed hair surgeons to raise the bar on FUE megasessions significantly above 1,500 FUs in one day. Vast numbers of FUE grafts in a single megasession have been reported.
Once again, a “race” started, with heroic, albeit foolishly extensive, FUE megasessions of several thousands of grafts extracted in a single sitting. These numbers initially applied only to the number of extracted and implanted grafts and did not consider transection rates, missed attempts, and final growth. That is a very different story making the safety of this practice extremely controversial.
Rassman et al. initially defined FUE megasessions as graft numbers that exceed 2,000 FUs in Caucasians with average hair density, in Asians on average 1,600 FUs, and for an African, anything above 1,200 FUs. They have also argued that there is a mathematical relationship determining a “safe FUE megasession”, which can be calculated by reducing a FUSS megasession by one-third. They consider that a human scalp can heal the number of grafts equal to two FUE megasessions over two or more sessions and that additional FUE harvesting is risky.
The risk behind FUE megasessions
In addition, as the number of harvested FUs increases and incisions are placed closer together in the limited space of the donor area, cumulative scalp microvasculature damage may appear.
Unfortunately, the vascular risks of FUE megasessions have been poorly documented. Many experts believe that vascular complications are far more common than reports indicate and that doctors ”hide” complications concerning vascular problems as related to wound healing, such as (a) the appearance of focal areas of scalp necrosis, (b) increased donor area miniaturization in the remaining hairs within the donor area after FUE. As the FUE megasession numbers rise, the injudicious harvesting of the finite donor supplies results in decimated, see-through, moth-eaten, thin donor areas. These are typical of indifferent operators, most often “nameless” technicians operating on unsuspected patients in low-cost FUE destinations.
FUE delegation and other ethical considerations
The boom of FUE is resulting mainly because of the advertisement done by the FUE machines marketing companies and black-market clinics. A smaller percentage is attributed to the advertising of neophyte doctors trying not to painstakingly learn techniques of dermatologic surgery.
The increased demand for FUE has led to an explosion of delegation of the harvesting step (or of the whole procedure) to non-physicians, who bear no responsibility for the damage they cause, under different sub-standard “working models”:
- The “Turnkey model”: an established doctor buys an FUE device from an instrument company, which also sends technicians to operate the device in his/her practice. The doctor “offers” FUE procedures under his name/brand but has no or minimal knowledge of the procedure whatsoever. Automated and robotic devices may fall into this category of “fly-in, fly-out” model of roving technicians, and the unethical use of these devices is one of the reasons that have led to the commoditization of FUE.
- The “Hair-Farm model”: one physician, not necessarily a hair surgeon, let alone an HR hair surgeon, supervises the various simultaneous surgeries done by the technicians. This is the new paradigm in many hugely advertised FUE destinations. The recent promotion of mechanized FUE appears to be encouraging techs/assistants to perform the whole FUE procedure under “physician supervision”. The delegation limits the doctor’s role to simply designing the hairline or welcoming the unsuspected patients in the clinic. In these facilities, unlicensed technicians will punch up more than 6,000 “grafts”, using tiny punches of 0.6mm to end-up with less than 2,000 non-fully transected grafts that they transplant along with the more than 4,000 extracted pieces of scalp skin. The overall result is typically poor, the donor area is totally wasted, and there is no possibility for future procedures due to depletion. This model can have numerous severe consequences to the well-being and physical health of patients who fall prey to these fraudulent clinics.
The “In-House Model”: staff members already within an experienced clinic team take over FUE harvesting or more steps of the procedure.
Conclusion
The official position of the ISHRS: “Comparison between Strip Harvesting and Follicular Unit Excision: A Fair and Balanced View. ISHRS Position Statement on Qualifications for Scalp Surgery”, summarizes most of the above details (quoting):
“No matter the technique employed, the hair surgeon must be well versed in the technical and aesthetic components of performing the surgery in order to produce consistently good results. A single course or training session on one aspect of the hair restoration procedure, such as harvesting, is inadequate training for a physician to learn how to perform hair restoration procedures. The surgeon must acquire a sense of the aesthetic and technical components of the procedure, and he or she must be able to develop a plan for patients with various clinical scenarios. All elements of HRS require considerable training and expertise to implement for each patient. Successful graft harvesting is only one small component of surgical hair restoration. Without attention to all of the other aspects, there is a very real possibility of a bad outcome. Finally, the incision of skin and tissue, whether using instruments that create a linear or circular incision, is legally considered surgery and should only be performed by a licensed physician with adequate training and expertise in hair restoration.”
Synopsis
FUE is an effective and useful modality for obtaining donor hair using manual, motorized, or robotic devices to remove individual follicular units from the donor region. The primary advantage over FUSS is the lack of a linear donor scar. Each extraction leaves a circular wound or incision, which heals with primary healing, leaving only a tiny scar. This is a significant advantage in patients who wish to wear their hair short and hide signs of surgery.
Over the past decades, FUE has become an increasingly popular HRS method, and the rising demand for FUE has driven the worldwide market size of HRS to an unprecedented height. Unfortunately, this is mostly due to the favorable appeal of false claims that FUE is “minimally invasive”, “scarless”, “painless” or “not even surgery”. Most patients opt-in for FUE due to these misconceptions, while many neophyte hair surgeons falsely believe that the learning curve of FUE is short just because the barrier of entry is low. FUE does actually have the advantage of no linear scar, but it carries several potential long-term side-effects and presents serious challenges for the physician. FUE reduces the overall density by “cherry-picking” of grafts, and to harvest the maximum amount of donor hair, FUs from areas of the scalp that are vulnerable to future hair loss are harvested. By creating maximum density in the frontal scalp, hair surgeons can paradoxically create thinning or see-through hair in the donor area.
Furthermore, there is the risk of a clinically apparent depletion of hair from the donor region, which creates an iatrogenic “moth-eaten” or “pseudo-syphilitic” appearance. Injuries on grafts are extremely easy to occur since FUE is a blind technique and can be minimized only with excellent technique, which takes years to master. All these problems are becoming alarmingly common due to the explosive rise of “black-market” clinics that offer FUE surgery performed by non-professional technicians on anyone willing to pay their low charge.
Even though recent technological advances have increased harvesting efficiency, the hair surgeon must have a thorough understanding of the nuances of FUE surgical technique to ensure consistent graft quality: the punch size, sharpness, composition, and design affect tissue cutting capabilities of punches, the quality of grafts, fluid dynamics of the follicle, tissue distortion, all must be decided on a patient-to-patient basis. The hair surgeon should be aware of the exact anatomy and physics behind FUE to achieve consistent results, and efficient FUE requires dexterity, training, dedication, devotion, enthusiasm, cognitive clarity, scientific knowledge, experience, and an extended learning curve. Physicians and patients who are aware of the short- and long-term risks of FUE are less likely to be disappointed when they occur. FUE is an invaluable addition in the armamentarium of an HR hair surgeon. The only point is its judicious use in the patients. The decision should be tailor-made.

Don’t hesitate to ask questions about the hair transplant technique you prefer. A specialized surgeon in Hair Transplant will gladly answer them.
Our opinion about FUE
At Anastasakis Hair Clinic, we have spent years perfecting the FUE technique to a level comparable to that of our FUT technique.
We are happy to help you explore your options and can provide you with a complete assessment free of charge and with no obligation. Send us some background information and your goals using our free online consultation form and we’ll provide your assessment, usually within 3 working days.
See some of the doctor’s hair transplant results, here.
















